To
learn about delivering healthcare in a resource limited setting. That's the
main objective of this training course in Blantyre, Malawi. I joked about this
before I left home: "I work in the NHS; I know all about limited
resources!". Little did I know.
I
was going to say my senses were assaulted on arrival to the hospital. That's
not quite true. What happened was much gentler. Overwhelmed, yes, but not
assaulted.
Walking
through the corridors of crumbling concrete, corrugated iron roofs and peeling
paint is like nowhere I've ever been. Looking out the windows into the various
courtyards I see lines and lines of colourful African print fabric drying in
the sunshine, families sitting chatting, meals being shared, children playing.
There are people everywhere but it's calm. There's a certain tranquility that
defies the crowds.
I
discover later that these people outside are waiting patiently for the next
visiting time so that they can tend to their loved ones, change sheets, provide
a meal. The fab
ric is the clean laundry, ready for the next bed change.
Through
a maze of corridors and walkways, we find the paediatric unit and are welcomed
by our host as a couple of chickens cluck outside the open window.
We're
divided into pairs and my buddy and I are dispatched to the neonatal unit where
we are met by a clinical officer. This is not a role I know, but during
the course of the day I learn that the unit could not survive without him.
There is little he doesn't know about caring for these tiny, vulnerable
infants. We join him on the first ward round of the day.
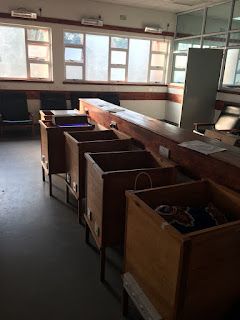 I'm
aware of a row of wooden boxes on legs lined up against the wall, and it takes
me a moment to realise that these are where the babies are nursed. On
closer inspection, I see that these boxes are specially made cots with rows of
light bulbs under the mattress to provide heat to these little babies. I
comment on the ingenuity of these bespoke cribs and am told "we just use
locally available materials". They're making do and it really works.
The babies are warm and cosy in brightly coloured traditional fabrics.
I'm
aware of a row of wooden boxes on legs lined up against the wall, and it takes
me a moment to realise that these are where the babies are nursed. On
closer inspection, I see that these boxes are specially made cots with rows of
light bulbs under the mattress to provide heat to these little babies. I
comment on the ingenuity of these bespoke cribs and am told "we just use
locally available materials". They're making do and it really works.
The babies are warm and cosy in brightly coloured traditional fabrics.
As
the round progresses, we see two babies who are both HIV and syphilis positive.
Now I'm outside the comfort zone. I haven't seen a patient with syphilis before
and I listen as our clinical officer patiently explains the treatment plan.
Blood cultures, antibiotics and feeding support. To this end, the mothers are
admitted to the ward every 2-3 hours to feed their baby and they do this with
great equanimity, either from the breast or via a nasogastric tube. There are
some chairs but not enough and some of them settle onto the floor with the baby
on their lap. Once feeding is done, they leave the ward and the babies sleep.
The
ward round progresses and we see babies with jaundice. Treatment plans are discussed.
I look around for phototherapy lamps and notice a small wooden box with
multiple LEDs embedded in it. Again, this is something made using the available
resources to meet a need. It's rested on the Perspex cot cover while the baby's
eyes are covered with a bandage to protect from the bright light.
Babies
are reviewed and moved to the Kangaroo Care area, where babies are nursed
skin-to-skin with their mothers before being ready for discharge. A couple of
babies are discharged and a plan made for "bench review". Is this a
new medical term? It's not something I've heard of. It becomes clear as our
next stop is the bench. It's a seating area outside the ward where babies are
reviewed daily or weekly to check progress. There's not really an appointment
but mothers wait their turn patiently. And this epitomises the feel of the
whole place. There is waiting, there is hoping and there is making do. All the
while there is acceptance and there is calm.
No comments:
Post a Comment